Beer Belly- Disproportional Fat Accumulation in the Belly Zone
The term “beer belly” is often used to describe the disproportionate accumulation of fat in the abdominal area. While excessive beer consumption is commonly blamed, underlying liver dysfunction and nutritional deficiencies can also contribute significantly to this condition.
This type of fat accumulation is not just a cosmetic concern but is associated with significant health risks, including metabolic syndrome, cardiovascular disease, and type 2 diabetes.
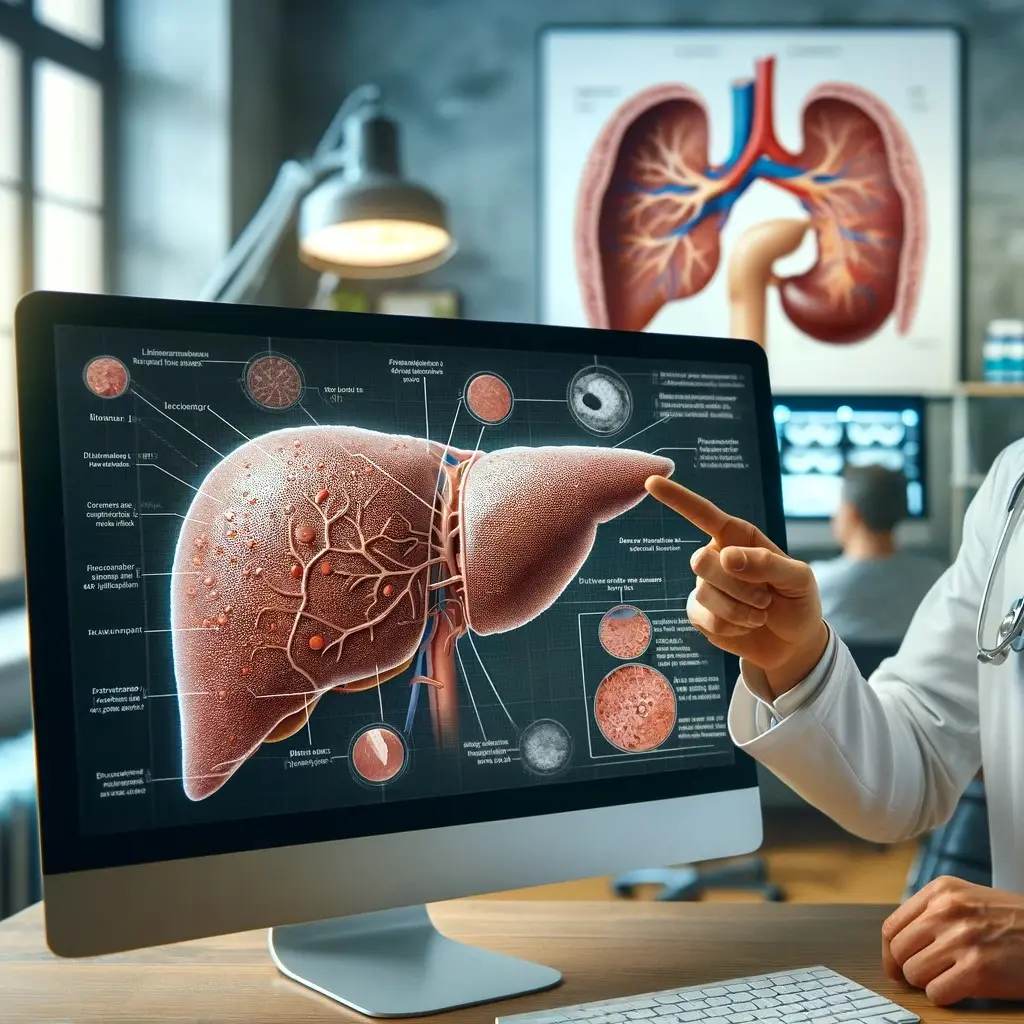
The liver is a central organ in regulating fat metabolism. It processes nutrients, detoxifies harmful substances, and plays a crucial role in lipid metabolism. When the liver is not functioning properly, it can lead to improper fat distribution, including the accumulation of visceral fat around the abdomen.
Key Nutrients for Liver Health
Choline:
- Function: Essential for liver function and lipid metabolism.
- Deficiency Impact: Leads to fat accumulation in the liver (hepatic steatosis) and impairs the liver’s ability to metabolize fats properly.
Inositol:
- Function: Plays a significant role in fat metabolism and insulin signaling.
- Deficiency Impact: Can result in poor lipid metabolism, contributing to fat buildup in the liver and abdominal area.
Methionine:
- Function: A vital amino acid necessary for methylation reactions and the synthesis of S-adenosylmethionine (SAMe), important for liver repair.
- Deficiency Impact: Impairs the liver’s detoxification processes and lipid metabolism, leading to fat accumulation.
Taurine:
- Function: An amino acid that aids in bile salt formation, detoxification, and protection against oxidative stress.
- Deficiency Impact: Affects bile production and liver detoxification, contributing to improper fat distribution and accumulation.
The Closed Loop Relationship
The relationship between nutrient deficiencies, fat accumulation in the liver (NAFLD), insulin resistance, and T2DM forms a closed loop, where each condition worsens the others.
Mechanisms of Interaction:
- Nutrient Deficiency: Lack of choline, inositol, methionine, and taurine disrupts normal liver function.
- Liver Dysfunction: Impaired liver function affects lipid metabolism and detoxification processes.
- Fat Accumulation: Disrupted lipid metabolism leads to fat buildup in the liver and visceral fat around the abdomen, manifesting as a “beer belly.”
Health Implications of a Beer Belly
The accumulation of visceral fat is associated with several serious health risks:
- Metabolic Syndrome: Includes conditions like hypertension, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels .
- Cardiovascular Disease: Higher risk of heart attack, stroke, and other cardiovascular conditions .
- Type 2 Diabetes: Higher likelihood of developing insulin resistance and T2DM .
- Liver Disease: Progression from non-alcoholic fatty liver disease (NAFLD) to non-alcoholic steatohepatitis (NASH), cirrhosis, and liver cancer .
Prevention and Management
Addressing nutrient deficiencies and improving liver health are crucial steps in preventing and managing abdominal fat accumulation:
- Dietary Adjustments: Ensure adequate intake of choline, inositol, methionine, and taurine through a balanced diet or via dietary supplements.
- Regular Exercise: Physical activity helps improve liver function and overall metabolic health.
- Limit Alcohol Consumption: Reducing alcohol intake can prevent further liver damage and fat accumulation.
A “beer belly” is not just a result of excessive beer consumption but can also indicate underlying liver dysfunction and nutritional deficiencies. Ensuring adequate intake of essential nutrients like choline, inositol, methionine, and taurine is vital for maintaining liver health and preventing disproportionate fat accumulation in the abdominal area.
LiverGuard delivers Choline, Inositol, Methionine, and Taurine in HIGH DOSE, supporting a fast and safe liver regeneration process, which will help you get rid of the beer belly.
References
- Zeisel, S. H., & da Costa, K. A. (2009). Choline: An Essential Nutrient for Public Health. Nutrition Reviews, 67(11), 615-623.
- Buchman, A. L., Sohel, M., Brown, M., Jenden, D. J., & Roch, M. (2001). The Effect of Choline Supplementation on Hepatic Steatosis in Patients Receiving Home Parenteral Nutrition. Hepatology, 34(3), 333-340.
- Beale, A., & Garcia-Perez, A. (2020). The Role of Inositol in the Treatment of Insulin Resistance. Clinical Therapeutics, 42(1), 63-72.
- Croze, M. L., & Soulage, C. O. (2013). Potential Role and Therapeutic Interests of Myo-Inositol in Metabolic Diseases. Biochimie, 95(10), 1811-1827.
- Finkelstein, J. D. (1990). Methionine Metabolism in Mammals. The Journal of Nutrition, 120(8), 1474-1477.
- Zeisel, S. H. (2006). Choline: Critical Role During Fetal Development and Dietary Requirements in Adults. Annual Review of Nutrition, 26, 229-250.
- Hayes, K. C., & Sturman, J. A. (1981). Taurine in Metabolism. Annual Review of Nutrition, 1, 401-425.
- Marcinkiewicz, J., & Kontny, E. (2014). Taurine and Inflammatory Diseases. Amino Acids, 46, 7-20.
- Cornier, M. A., Dabelea, D., Hernandez, T. L., Lindstrom, R. C., Steig, A. J., Stob, N. R., Van Pelt, R. E., Wang, H., & Eckel, R. H. (2008). The Metabolic Syndrome. Endocrine Reviews, 29(7), 777-822.
- Grundy, S. M., Cleeman, J. I., Daniels, S. R., Donato, K. A., Eckel, R. H., Franklin, B. A., Gordon, D. J., Krauss, R. M., Savage, P. J., Smith, S. C. Jr., Spertus, J. A., & Costa, F. (2005). Diagnosis and Management of the Metabolic Syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation, 112(17), 2735-2752.
- DeFronzo, R. A., Ferrannini, E., Zimmet, P., & Alberti, G. (2015). International Textbook of Diabetes Mellitus, 4th Ed. Wiley-Blackwell.
- Targher, G., Corey, K. E., Byrne, C. D., & Roden, M. (2021). The Complex Link between NAFLD and Type 2 Diabetes Mellitus — Mechanisms and Treatments. Nature Reviews Gastroenterology & Hepatology, 18(9), 599-612.
- Kawanaka, M., Nishino, K., Nakamura, J., Urata, N., & Oka, T. (2021). Nutrient Deficiencies in Patients with Non-Alcoholic Fatty Liver Disease. Clinical Nutrition ESPEN, 41, 249-256.
- World Health Organization. (2020). WHO Guidelines on Physical Activity and Sedentary Behaviour.
- Poppitt, S. D. (2015). Beverage Consumption: Are Alcoholic and Sugary Drinks Tipping the Balance towards Overweight and Obesity? Nutrition Bulletin, 40(2), 166-177.
- Day, C. P. (2006). From Fat to Inflammation. Gastroenterology, 130(1), 207-210.