Fat in the human body serves several critical functions, from storing energy to cushioning vital organs. However, not all fat is created equal. While many of us are aware of the fat that lies just beneath our skin, known as subcutaneous fat, there is another, less visible type of fat that can be far more dangerous: liver fat. Even a small increase in fat within the liver can have serious health consequences, making it crucial to understand how to manage this often-overlooked issue.
Types of Fat in the Body
In an average man who is 175 cm tall and weighs 75 kg, fat is distributed in several key areas:
- Subcutaneous Fat: This is the fat stored just under the skin and makes up about 80-90% of total body fat, amounting to roughly 9 to 13.5 kg. It serves as insulation and protection for the body.
- Visceral Fat: Found around internal organs like the liver and intestines, visceral fat is more dangerous than subcutaneous fat. It accounts for about 10-20% of total body fat, or approximately 1.1 to 3 kg.
- Intramuscular Fat: This fat is stored within muscles and comprises about 5-10% of total body fat, or 0.5 to 1.5 kg. It serves as an energy reserve during exercise.
- Liver Fat: Fat stored within the liver, ideally less than 5% of the liver’s weight. For a liver that weighs 1.5 to 2 kg, this translates to just 75 to 100 grams of fat.
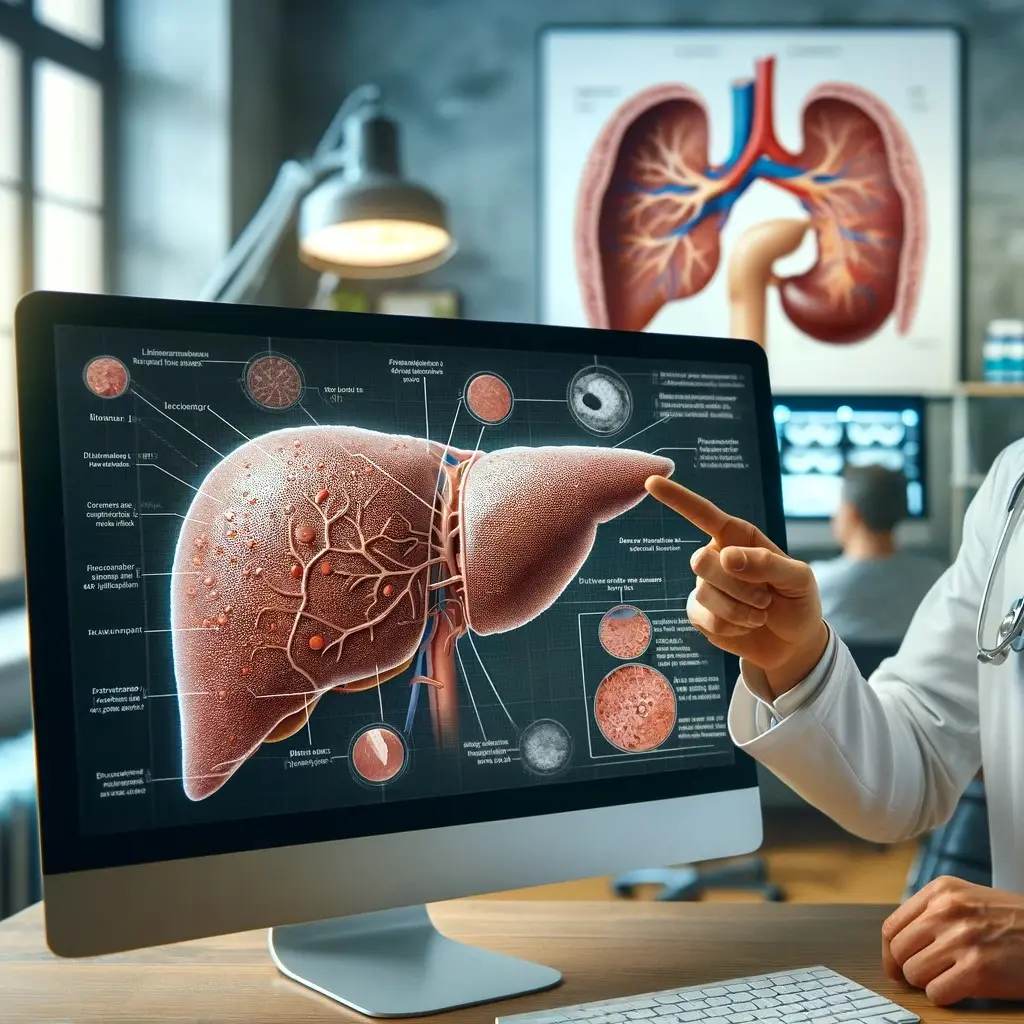
The Danger of Excess Liver Fat
While it’s normal to have a small amount of fat in the liver, even a slight increase can lead to serious health issues. When the liver’s fat content exceeds 5%, it results in Non-Alcoholic Fatty Liver Disease (NAFLD). For a man of average size, this means that just an additional 100 grams of fat in the liver can push it into the dangerous territory.
NAFLD is not just a minor inconvenience. It impairs the liver’s ability to perform its essential functions, including detoxifying the blood, producing bile for digestion, and managing glucose and fat metabolism. As the liver becomes increasingly fatty, it can lead to inflammation and progress to a more severe condition called non-alcoholic steatohepatitis (NASH). NASH can further develop into cirrhosis, liver failure, or liver cancer.
What makes NAFLD particularly alarming is that it often shows no symptoms until significant damage has occurred. By the time symptoms like fatigue, abdominal discomfort, or jaundice appear, the liver may already be severely compromised.
How Much Fat Needs to Be Removed?
To return a fatty liver to a healthy state, the goal is to reduce the liver fat content to less than 5% of the liver’s weight. For an average man, this means the liver fat should be reduced to 75-100 grams. If the liver has accumulated more fat—say, 150 to 400 grams—this means removing anywhere from 50 to 300 grams of fat to restore normal liver function.
Standard Approach for Fatty Liver Removal: Diet and Lifestyle Changes
The most common method for reducing liver fat involves diet and lifestyle modifications. These typically include:
- Caloric Restriction: Reducing overall calorie intake to promote weight loss.
- Low-Carbohydrate Diet: Minimizing the intake of sugars and refined carbohydrates, which can contribute to fat accumulation in the liver.
- Increased Physical Activity: Engaging in regular exercise to burn fat and improve liver function.
This approach can be quite restrictive. It often requires individuals to significantly alter their eating habits, cutting out many foods they enjoy. The strictness of this diet can make it difficult to adhere to over the long term, potentially leading to frustration and relapse. Unfortunately, most people fail to follow this regiment long enough to see tangible results.
A Less Restrictive Approach: Essential Nutrients for Liver Health
Fortunately, there are nutrients that can help reduce liver fat without the need for a highly restrictive diet. These include:
- Choline prevents fat accumulation by helping to transport fats out of the liver.
- Inositol improves insulin sensitivity and regulates lipid metabolism, reducing the liver’s fat burden.
- Methionine supports detoxification and lipid metabolism, aiding in the removal of fats from the liver.
- Taurine improves fat digestion through bile acid conjugation and protects the liver from oxidative damage.
Incorporating these nutrients into your diet can provide significant benefits in reducing liver fat without the need for drastic dietary changes.
LiverGuard is specifically formulated with this goal in mind. Provide you with the proper amount of those essential nutrients, so you can give your liver a chance to release the accumulated fat, without the restrictive diet. LiverGuard gives the people the option to have more manageable way to support liver health and prevent the progression of NAFLD.
Conclusion
Liver fat, even in small amounts, poses significant health risks. Just an additional 100 grams of fat can push the liver into a diseased state, leading to conditions that are difficult to reverse and may have serious, long-term consequences. Traditional approaches to reducing liver fat often require restrictive diets that can be challenging to maintain. However, by incorporating essential nutrients like choline, inositol, methionine, and taurine into your diet, you can help manage liver fat more effectively and comfortably. Protecting your liver is critical, and understanding the impact of liver fat is the first step toward better health.
References
- Farrell, G. C., & Larter, C. Z. (2006). Nonalcoholic Fatty Liver Disease: From Steatosis to Cirrhosis. Hepatology, 43(S1), S99-S112. https://doi.org/10.1002/hep.20973
- Rinella, M. E. (2015). Nonalcoholic Fatty Liver Disease: A Systematic Review. JAMA, 313(22), 2263-2273. https://doi.org/10.1001/jama.2015.5370
- Chalasani, N., Younossi, Z., Lavine, J. E., Diehl, A. M., Brunt, E. M., Cusi, K., … & Sanyal, A. J. (2012). The diagnosis and management of non‐alcoholic fatty liver disease: Practice Guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Hepatology, 55(6), 2005-2023. https://doi.org/10.1002/hep.25762
- Zeisel, S. H. (2006). Choline: Critical Role During Fetal Development and Dietary Requirements in Adults. Annual Review of Nutrition, 26(1), 229-250. https://doi.org/10.1146/annurev.nutr.26.061505.111156
- Michell, R. H. (2008). Inositol derivatives: Evolution and functions. Nature Reviews Molecular Cell Biology, 9(2), 151-161. https://doi.org/10.1038/nrm2334
- Brosnan, J. T., & Brosnan, M. E. (2006). The Sulfur-Containing Amino Acids: An Overview. The Journal of Nutrition, 136(6), 1636S-1640S. https://doi.org/10.1093/jn/136.6.1636S
- Schaffer, S. W., & Jong, C. J. (2010). Taurine: A Diet-Derived Antioxidant in the Prevention and Treatment of Cardiovascular Disease. Current Opinion in Clinical Nutrition and Metabolic Care, 13(6), 644-651. https://doi.org/10.1097/MCO.0b013e32833e8c03