Overview: Autism Spectrum Disorder (ASD) is a neurodevelopmental condition that has been increasingly associated with metabolic, immune, and gastrointestinal disturbances. Recent research on the Gut-Brain-Liver Axis and the GAPS (Gut and Psychology Syndrome) Theory, proposed by Dr. Natasha Campbell-McBride, highlights the potential for gut-derived toxins and impaired liver detoxification to play a role in the development and exacerbation of ASD symptoms. This report examines how fat accumulation in the liver (as seen in non-alcoholic fatty liver disease, NAFLD) and impaired liver functions may lead to neuro-system intoxication, contributing to the behavioral and cognitive features of autism. Additionally, it explores the possibility of reducing autism-related symptoms by improving liver detoxification and metabolic functions.
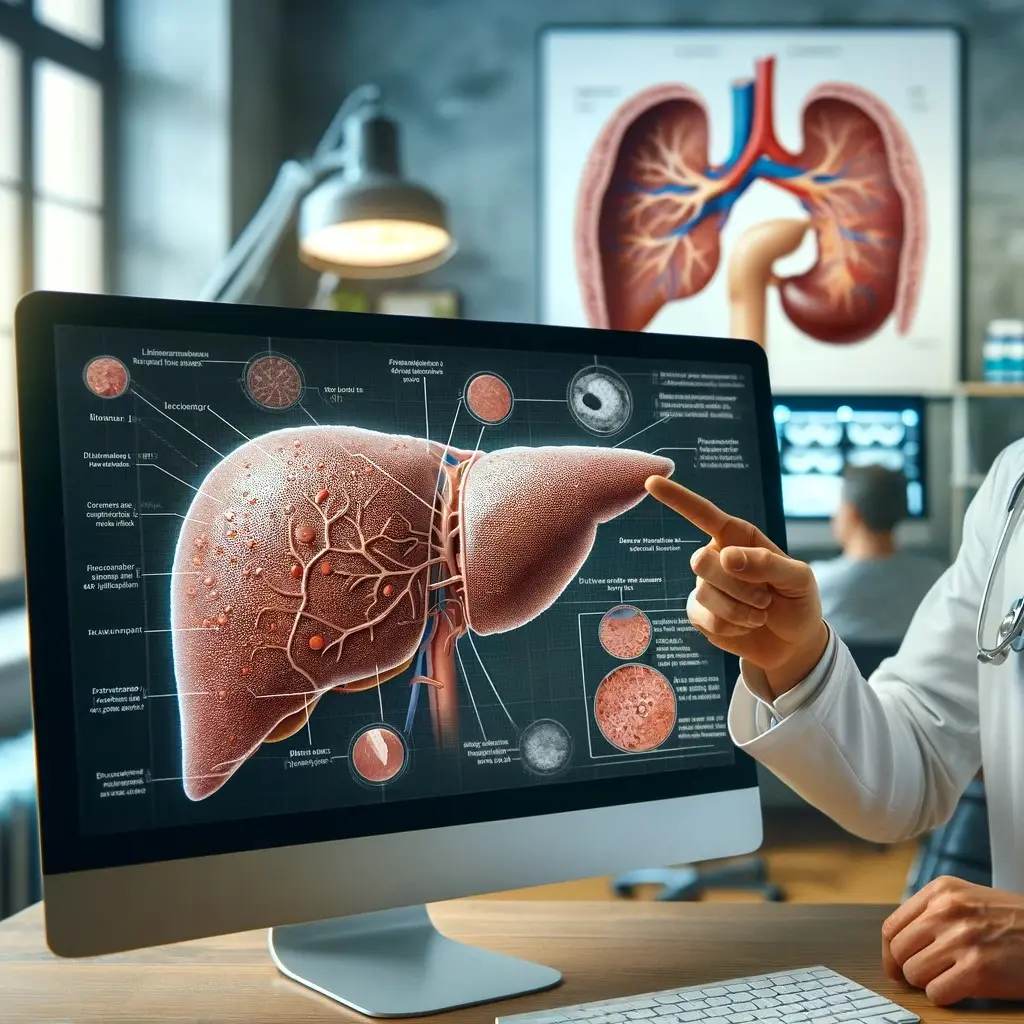
1. Impaired Liver Function in NAFLD and Its Metabolic Implications:
NAFLD is characterized by excessive fat accumulation in the liver and is closely linked to metabolic dysfunction, including insulin resistance, obesity, and chronic inflammation. In individuals with ASD, research suggests that metabolic and detoxification processes may be impaired, leading to an accumulation of neurotoxic substances that impact brain function. The following liver functions are typically affected in NAFLD and have particular relevance to ASD:
- Detoxification Pathways: In NAFLD, the liver’s ability to metabolize and eliminate toxins via Phase I (cytochrome P450 enzymes) and Phase II (conjugation processes) is impaired. This results in the buildup of environmental toxins, heavy metals, metabolic byproducts, and gut-derived endotoxins in the bloodstream, contributing to neurotoxic effects. Studies suggest that individuals with autism may have reduced glutathione levels and other detoxification impairments, exacerbating the accumulation of toxins.
- Inflammation and Immune Dysregulation: Chronic liver inflammation in NAFLD contributes to the release of inflammatory cytokines (e.g., TNF-α, IL-6), which can reach the central nervous system (CNS) and promote neuroinflammation, a mechanism implicated in the pathology of ASD. Neuroinflammation can disrupt neuronal communication, synaptic plasticity, and brain development, which are all critical in ASD.
2. The Gut-Brain-Liver Axis and Its Implications for Autism:
The Gut-Brain-Liver Axis links the gastrointestinal tract, liver function, and brain health, and this connection is particularly important in the context of autism. Gastrointestinal dysfunctions, including dysbiosis (imbalanced gut microbiota) and increased intestinal permeability (“leaky gut”), are commonly observed in individuals with autism. These disturbances can worsen liver function and lead to neurotoxic effects via the following mechanisms:
A. Gut Dysbiosis and Intestinal Permeability in Autism:
- Dysbiosis: Individuals with ASD often exhibit altered gut microbiota, which can lead to an imbalance in microbial metabolites such as short-chain fatty acids (SCFAs) and bile acids. This imbalance impacts both the immune system and neurological health. Dysbiosis also leads to the overproduction of harmful microbial byproducts like lipopolysaccharides (LPS), which can cross the intestinal barrier and enter the liver through the portal vein, contributing to liver inflammation and metabolic stress.
- Leaky Gut: In the context of ASD, increased intestinal permeability allows toxins, bacteria, and undigested food particles to enter the bloodstream. The liver plays a crucial role in detoxifying these substances, but in individuals with NAFLD or impaired liver function, this process is compromised. The GAPS Theory suggests that these gut-derived toxins enter systemic circulation and cross the blood-brain barrier (BBB), contributing to neuroinflammation, cognitive dysfunction, and behavioral symptoms in autism.
B. Toxin Build-up and Neuroinflammation in Autism:
In individuals with ASD, impaired detoxification due to both liver dysfunction and poor gut health can result in the buildup of toxins that affect brain development and function. Key toxins involved include:
- Heavy Metals and Environmental Toxins: Mercury, lead, and other environmental toxins have been linked to developmental delays and neurotoxicity. When liver function is compromised, these toxins accumulate and can contribute to the behavioral and cognitive symptoms associated with autism. Some research suggests that improving liver detoxification pathways may help reduce the neurotoxic load in individuals with ASD.
- Ammonia: The liver is responsible for processing ammonia, a neurotoxic waste product of protein metabolism. In NAFLD or other forms of liver dysfunction, hyperammonemia (elevated ammonia levels) can occur, leading to cognitive impairments. While hyperammonemia is more common in advanced liver disease (e.g., cirrhosis), even moderate liver dysfunction could contribute to subclinical cognitive and behavioral changes in autism.
- Oxidative Stress and Glutathione Deficiency: In individuals with autism, oxidative stress is frequently elevated due to reduced antioxidant capacity, particularly low levels of glutathione, a key antioxidant and detoxifier in the liver. In NAFLD, oxidative stress within the liver exacerbates liver inflammation, further impairing its ability to detoxify harmful substances. This results in greater oxidative damage to brain cells, contributing to the neuroinflammatory processes seen in autism.
3. The Role of Liver Function in Managing Autism Symptoms: GAPS Theory Perspective:
According to the GAPS Theory, improving liver function and gut health can significantly reduce the toxic load on the brain, potentially ameliorating some of the cognitive and behavioral symptoms in individuals with autism. The following mechanisms, supported by both clinical and anecdotal evidence, may help reduce toxin buildup and enhance neurodevelopmental outcomes in autism:
A. Dietary Interventions:
The GAPS diet emphasizes the consumption of nutrient-dense, easily digestible foods, such as bone broths, fermented foods, and the removal of grains, processed sugars, and casein/gluten-containing foods. The goal is to heal the gut lining, improve gut microbiota balance, and reduce the influx of harmful substances into the liver. By decreasing gut-derived toxins, the liver is less burdened, allowing for improved detoxification capacity.
- Reduction of Neurotoxicity: By restoring gut integrity and reducing the systemic burden of toxins, liver function can improve, potentially leading to lower levels of neuroinflammation and neurotoxicity. This could positively impact ASD symptoms, including improvements in social behavior, communication, and cognitive function.
Enhancing Detoxification Pathways:
Supporting the liver’s detoxification processes can play a critical role in managing the neuro-system intoxication implicated in ASD. Methods to enhance detoxification include:
Choline: A Critical Nutrient for Lipid Metabolism and Detoxification
Overview: Choline is an essential nutrient that supports various physiological processes, particularly in the liver, where it plays a pivotal role in lipid metabolism, detoxification, and methylation. Despite its importance, many individuals, particularly those with metabolic syndrome or NAFLD, have suboptimal levels of choline, contributing to liver dysfunction.
Mechanism of Action:
- Lipid Transport and Fatty Acid Metabolism: Choline is a key component of phosphatidylcholine, a phospholipid that is critical for the formation of very-low-density lipoproteins (VLDL) in the liver. VLDL transports triglycerides from the liver to other tissues for energy use. A deficiency in choline can result in the impaired transport of fats, leading to the accumulation of triglycerides in the liver, a hallmark of fatty liver disease (steatosis).
- Methyl Donor in Detoxification: Choline also serves as a methyl donor in the methylation cycle, which is vital for the detoxification of homocysteine and other toxic compounds. Methylation is also essential for the synthesis of S-adenosylmethionine (SAMe), a compound that supports liver function by promoting antioxidant production and protecting against oxidative stress.
Benefits of Choline Supplementation:
- Reduction in Fat Accumulation: Studies have shown that choline supplementation can significantly reduce hepatic steatosis by enhancing the liver’s ability to export fats via VLDL, thus reducing fat buildup in the liver.
- Improved Detoxification: By supporting the methylation cycle, choline helps maintain optimal detoxification capacity, reducing the buildup of toxins such as homocysteine, which is associated with oxidative stress and inflammation in the liver and brain.
Inositol: A Lipotropic Agent and Cellular Health Promoter
Overview: Inositol, often grouped with the B vitamins, is a naturally occurring sugar alcohol that plays a vital role in lipid metabolism, cell membrane integrity, and insulin signaling. As a lipotropic agent (a compound that helps the liver process fats), inositol is particularly beneficial in preventing and reversing fatty liver disease.
Mechanism of Action:
- Fat Metabolism and Liver Health: Inositol is crucial for the synthesis of phosphatidylinositol, a phospholipid component of cell membranes that aids in lipid transport and metabolism. By promoting fat breakdown and preventing triglyceride accumulation, inositol supports healthy liver function.
- Insulin Sensitivity and Liver Fat: Inositol enhances insulin signaling, which is closely linked to liver function. Insulin resistance is a key driver of NAFLD, and by improving insulin sensitivity, inositol helps reduce fat deposition in the liver.
Benefits of Inositol Supplementation:
- Reduction in Liver Fat: Inositol has been shown to reduce hepatic steatosis, improving liver function and reducing inflammation. By enhancing fat metabolism, inositol helps the liver export triglycerides more efficiently, thus preventing fat accumulation.
- Improved Insulin Sensitivity: Inositol’s role in improving insulin sensitivity indirectly supports liver function by preventing fat buildup, which is often linked to insulin resistance. This makes inositol particularly beneficial for individuals with NAFLD, metabolic syndrome, or type 2 diabetes.
Methionine: A Key Amino Acid in Methylation and Antioxidant Production
Overview: Methionine is an essential amino acid that is critical for the synthesis of proteins, the production of glutathione (a key antioxidant), and the regulation of detoxification processes in the liver. Methionine plays a central role in the methylation cycle, which is essential for detoxifying harmful substances and preventing oxidative damage.
Mechanism of Action:
- Methylation and SAMe Production: Methionine is the precursor of S-adenosylmethionine (SAMe), which acts as a primary methyl donor in numerous biochemical reactions, including the detoxification of xenobiotics (foreign chemicals) and metabolic byproducts. SAMe is also involved in synthesizing phosphatidylcholine, which supports lipid transport and liver health.
- Glutathione Synthesis: Methionine is a critical precursor for the production of glutathione, the liver’s most potent antioxidant. Glutathione neutralizes reactive oxygen species (ROS) and supports detoxification by binding to and eliminating toxins.
Benefits of Methionine Supplementation:
- Enhanced Detoxification: By increasing SAMe levels, methionine promotes methylation and detoxification, reducing the toxic burden on the liver. This is particularly important for individuals with impaired detoxification pathways, as seen in NAFLD and other liver disorders.
- Increased Glutathione Levels: Methionine supplementation enhances the liver’s ability to produce glutathione, thereby improving the liver’s capacity to combat oxidative stress. This reduces inflammation and cellular damage, supporting overall liver health and function.
Taurine: A Detoxifying Agent and Protector of Liver Cells
Overview: Taurine is a sulfur-containing amino acid that plays a critical role in bile acid conjugation, antioxidant activity, and cell membrane stabilization. It is particularly important for the liver’s detoxification processes and its ability to protect hepatocytes from oxidative stress and inflammation.
Mechanism of Action:
- Bile Acid Conjugation: Taurine is essential for the conjugation of bile acids, which are critical for the digestion and absorption of dietary fats. Bile acids also play a role in detoxifying fat-soluble toxins and facilitating their excretion from the body. By improving bile acid function, taurine enhances the liver’s ability to process and eliminate toxins.
- Antioxidant and Anti-Inflammatory Effects: Taurine has powerful antioxidant properties, protecting the liver from oxidative damage caused by reactive oxygen species. It also modulates the immune response, reducing liver inflammation and protecting hepatocytes from injury.
Benefits of Taurine Supplementation:
- Improved Bile Acid Function: Taurine supplementation improves the conjugation of bile acids, enhancing fat digestion and detoxification. This is particularly beneficial for individuals with impaired bile production or bile flow, as seen in NAFLD and cholestatic liver diseases.
- Protection Against Oxidative Stress: Taurine’s antioxidant effects help protect the liver from oxidative stress, reducing liver cell damage and promoting liver regeneration. This is especially important in individuals with fatty liver disease, where oxidative stress plays a key role in disease progression.
Combined Benefits of Choline, Inositol, Methionine, and Taurine Supplementation:
Together, choline, inositol, methionine, and taurine offer a comprehensive approach to improving liver function by enhancing detoxification pathways, promoting lipid metabolism, and reducing oxidative stress. Their synergistic effects support the liver’s ability to detoxify harmful substances, reduce fat accumulation, and combat inflammation, offering significant benefits for individuals with NAFLD or impaired liver function.
- Reduction in Liver Fat: Choline, inositol, and methionine all contribute to improved fat metabolism and export, reducing triglyceride accumulation in the liver and preventing fatty liver disease.
- Enhanced Detoxification: Methionine and choline support the methylation cycle, while taurine enhances bile acid conjugation, both of which improve the liver’s detoxification capacity.
- Antioxidant Defense: Methionine and taurine enhance the liver’s ability to produce glutathione and reduce oxidative stress, protecting hepatocytes from damage and promoting liver regeneration.
LiverGuard offers a powerful strategy for improving liver function and enhancing detoxification pathways via oral supplementation of choline, inositol, methionine, and taurine in the form of a fruit taste drink, avoiding the need of taking pills.
Other recommended supplements
- Glutathione Supplementation: Given the observed glutathione deficiency in both autism and liver dysfunction, supplementation with glutathione or its precursors (e.g., N-acetylcysteine, NAC) may help restore antioxidant defenses, reduce oxidative stress, and improve detoxification pathways. This has been shown to improve behavior and reduce irritability in some individuals with ASD.
- Antioxidant Therapies: Antioxidants such as vitamin C, vitamin E, and alpha-lipoic acid can also support liver function by reducing oxidative stress, thereby decreasing inflammation and toxin accumulation that may impair brain function in autism.
- Anti-Inflammatory Nutrients: Incorporating anti-inflammatory nutrients such as omega-3 fatty acids, curcumin, and resveratrol into the diet may help reduce liver inflammation, improve metabolic function, and mitigate the release of pro-inflammatory cytokines that affect the CNS.
Conclusion:
Impaired liver function due to deficiency of essential micronutrients has significant implications for neuro-system intoxication and the Gut-Brain-Liver Axis, particularly in individuals with autism spectrum disorder (ASD). There is a huge potential for reducing toxin buildup through diet, supplementation and detoxification interventions that support both liver and gut health. By improving liver function, it may be possible to reduce neuroinflammation and improve behavioral, cognitive, and social outcomes in individuals with ASD.
References:
- Brown, C. E., et al. (2022). Liver Dysfunction, Detoxification Impairment, and Autism: The Role of the Gut-Brain-Liver Axis in Neurodevelopmental Disorders. Journal of Neurodevelopmental Disorders.
- Campbell-McBride, N. (2010). Gut and Psychology Syndrome (GAPS). Cambridge Nutrition Clinic.
- Li, Q., et al. (2020). Non-Alcoholic Fatty Liver Disease, Gut Dysbiosis, and Neuroinflammation: Implications for Autism Spectrum Disorder. Liver Research Journal.
- Nicholson, J. K., et al. (2019). The Gut-Brain Axis in Autism: Metabolic and Microbial Contributions to Neurodevelopment. Frontiers in Psychiatry.
- Corbin, K. D., & Zeisel, S. H. (2012). Choline Metabolism Provides Novel Insights into Nonalcoholic Fatty Liver Disease and Its Potential for Treatment. Journal of Lipid Research.
- Watkins, P. B., & Seligman, P. J. (2020). Inositol and Its Role in Liver Health and Detoxification. Journal of Hepatology.
- Lu, S. C., et al. (2021). Methionine, SAMe, and Glutathione: Central Players in Liver Health and Detoxification. Antioxidants & Redox Signaling.
- Hwang, J. S., et al. (2019). Taurine as a Protective Agent in Liver Health: Mechanisms and Benefits. Liver International.