Introduction
Fatty liver disease (FLD) is a spectrum of liver disorders characterized by the accumulation of excess fat in the liver. FLD is increasingly recognized as the most common liver disorder in industrialized nations, closely linked to metabolic syndrome, obesity, type 2 diabetes, and dyslipidemia.
FLD has emerged as the leading cause of chronic liver disease worldwide, affecting approximately 40% of the global population aging over 35. The prevalence is significantly higher in individuals with obesity and diabetes, reaching up to 70-90% in these populations. The incidence of FLD is increasing, paralleling the global rise in obesity and type 2 diabetes. FLD affects both adults and children, with a growing concern for its impact on pediatric populations.
Pathogenesis
The pathogenesis of FLD is multifactorial and complex, involving a combination of genetic, environmental, and metabolic factors. The widely accepted “two-hit” hypothesis has been replaced by a more nuanced “multiple-hit” model. This model suggests that various factors act synergistically to promote liver fat accumulation and inflammation.
- Deficiency of micronutrients: It is already ultimately proven, that the deficiency of Choline (classified sometimes as a vitamin, belonging to the group of B vitamins), does cause FLD, the same way like deficiency of vitamin C causes scurvy.
- Dysregulation of Hepatic Glucose Production: The liver plays a key role in maintaining glucose homeostasis by balancing glucose production and storage. In a healthy liver, insulin suppresses gluconeogenesis (the production of glucose). However, in the presence of fatty liver, this suppression becomes impaired, leading to increased hepatic glucose output despite elevated insulin levels, contributing to systemic insulin resistance.
- Insulin resistance: Central to the pathogenesis of FLD, insulin resistance promotes lipolysis in adipose tissue, leading to increased free fatty acid (FFA) influx into the liver. The liver, unable to fully metabolize these FFAs, accumulates triglycerides.
This is how FLD and Insulin resistance close a self-perpetuating cycle, which can be broken either by eliminating “the fuel”– all kind of carbohydrates, or by eliminating the root cause- the micronutrient deficiency. By providing the liver with Choline and several other micronutrients like methionine, inositol and taurine, it can drop the extra fat accumulated and start to regenerate.
What is Causing Those Micronutrient Shortages?
1. Increased Demand of the Liver, for Catalysts (vitamins) and Reagents (minerals and amino acids) for its detoxification functions, resulting from increased volumes of toxins, which need to be methylated (deactivated and extracted from the body), delivered by food, water and air.
2. Reduced Nutrient Density: Modern agricultural practices have significantly increased crop yields, producing 7-8 times more harvests per season from the same land through the use of artificial fertilizers, primarily containing nitrogen (N), phosphorus (P), and potassium (K). While this boosts the size and mass of the plants, it results in crops that are primarily composed of energy but contain significantly fewer essential micronutrients. Depending on the specific nutrient and crop, studies proved 10- 40% less microelements compared to those grown in the past. This includes reductions in essential micronutrients (like iron, zinc, and magnesium) and vitamins (such as vitamin C) in modern crops This phenomenon is often referred to as the dilution effect.
3. The damage caused on the Gut microbiota: can significantly impair the body’s ability to absorb essential micronutrients such as vitamins and minerals. The gut microbiota plays a crucial role in breaking down food, synthesizing vitamins and assisting in the absorption of minerals. Disruption of this microbial balance, often due to poor diet and antibiotics, or chronic illness, can lead to malabsorption. This reduction in nutrient uptake can contribute to deficiencies, affecting overall health, immunity, and metabolic function.
In short, compared to 60-70 years ago, even with the same amount of food, we have less microelements, which are absorbed at a lower rate, while at the same time we have increased demands due to the increasing toxicity in the environment, water and food. This is how we end up with Choline shortages leading to fat accumulation in the liver (FLD).
This all gets worsen by a variety of factors like:
Oxidative stress: Excess FFAs undergo oxidation in hepatocytes, generating reactive oxygen species (ROS), which damage cellular structures and exacerbate inflammation.
Gut microbiota and endotoxins: Dysbiosis, or an imbalance in gut microbiota, may lead to increased intestinal permeability, allowing endotoxins (e.g., lipopolysaccharides) to enter the circulation and contribute to liver inflammation.
Genetic factors: Polymorphisms in genes such as PNPLA3, TM6SF2, and MBOAT7 have been associated with increased susceptibility to NAFLD and its progression
Clinical Manifestations
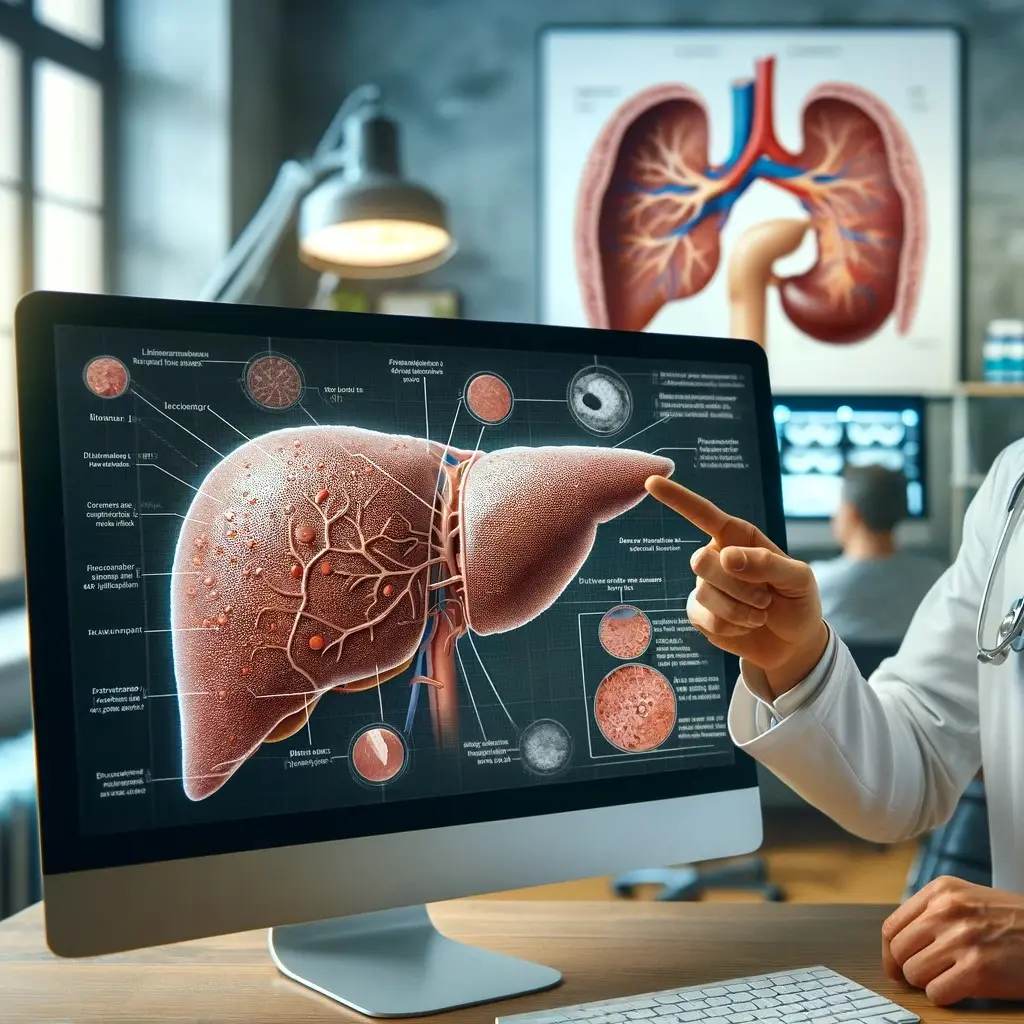
FLD is a silent disease, often asymptomatic in its early stages. It encompasses a spectrum ranging from simple steatosis (non-alcoholic fatty liver, NAFL) to non-alcoholic steatohepatitis (NASH), which can progress to cirrhosis and hepatocellular carcinoma (HCC).
- Non-alcoholic fatty liver (NAFL): Characterized by the accumulation of fat in hepatocytes without significant inflammation or fibrosis. It is generally considered benign but can progress to NASH.
- Non-alcoholic steatohepatitis (NASH): Involves hepatocellular inflammation and varying degrees of fibrosis. NASH poses a higher risk of progression to cirrhosis and HCC.
- Cirrhosis and hepatocellular carcinoma (HCC): In some cases, NASH progresses to cirrhosis, characterized by extensive fibrosis, impaired liver function, and increased risk of developing HCC.
Diagnostic Approaches
The diagnosis of FLD is typically based on clinical evaluation, blood samples and imaging studies.
Imaging: Ultrasonography is the most commonly used imaging modality for detecting hepatic steatosis. More advanced techniques, such as transient elastography (FibroScan) and magnetic resonance imaging-proton density fat fraction (MRI-PDFF), provide valuable information about liver stiffness and fat content.
- Biomarkers: Several serum biomarkers and scoring systems, such as the NAFLD fibrosis score (NFS), FIB-4, and AST-to-platelet ratio index (APRI), can help assess the severity of fibrosis and the likelihood of NASH.
- Liver biopsy: Although invasive, liver biopsy is the only definitive method for distinguishing between simple steatosis and NASH and for staging fibrosis.
Management and Treatment
The management of FLD focuses on treating the underlying metabolic disorders and preventing disease progression. Although no specific pharmacotherapy for FLD has been approved, Choline supplementation (like LiverGuard), is the way to prevent and reduce liver fat accumulation, as per EFSA (European Food Safety Authority).
Weight loss through dietary changes and physical activity can be beneficial for the liver and overall health, especially in obese patients.
Prognosis and Complications
Though hepatic steatosis alone may not result in overt liver dysfunction, it creates a metabolic environment conducive to further liver and overall health injury.
Complications
Oxidative Stress and Mitochondrial Dysfunction
The accumulation of free fatty acids (FFAs) in hepatocytes leads to increased fatty acid oxidation, generating reactive oxygen species (ROS). ROS production overwhelms the liver’s antioxidant defenses, resulting in oxidative stress, causing Mitochondrial Damage and Lipid Peroxidation.
Key Liver Functions Suppressed by Liver Fat Accumulation
The accumulation of fat in the liver disrupts several critical hepatic functions:
- Glucose Metabolism:
- Gluconeogenesis and Glycogen Storage: Hepatic steatosis impairs glucose regulation, contributing to hyperglycemia and increasing the risk of type 2 diabetes mellitus (T2DM).
- Lipid Metabolism:
- VLDL Secretion: Decreased export of triglycerides exacerbates hepatic fat accumulation, promoting systemic dyslipidemia (increased serum triglycerides and reduced HDL cholesterol).
- Detoxification:
- Ammonia Clearance: Impaired urea cycle function in advanced NAFLD can lead to hyperammonemia, resulting in hepatic encephalopathy.
- Drug Metabolism: The liver’s ability to detoxify xenobiotics is compromised, increasing susceptibility to drug toxicity and adverse reactions.
- Protein Synthesis:
- Clotting Factors and Albumin: Reduced synthesis of coagulation proteins increases the risk of bleeding, while decreased albumin production contributes to edema and ascites.
- Bile Production:
- Fat Digestion and Vitamin Absorption: Impaired bile secretion reduces the absorption of fat-soluble vitamins (A, D, E, K), leading to deficiencies.
Systemic Consequences of FLD
While the liver is the primary organ affected in FLD, fat deposition and the resultant inflammatory and metabolic disruptions have widespread consequences beyond the liver.
1. Cardiovascular Disease (CVD)
FLD is closely associated with cardiovascular diseases, which represent the leading cause of mortality in FLD patients. Key mechanisms include:
- Atherosclerosis: Systemic inflammation, oxidative stress, and dyslipidemia promote endothelial dysfunction and plaque formation in arteries.
- Hypertension and Heart Failure: Elevated blood pressure and impaired cardiac function are common in advanced FLD.
2. Type 2 Diabetes Mellitus (T2DM)
Insulin resistance is central to the pathogenesis of FLD, and as the disease progresses, it exacerbates systemic insulin resistance, increasing the risk of developing T2DM. Hepatic insulin resistance further impairs glucose metabolism, creating a vicious cycle between FLD and diabetes.
3. Chronic Kidney Disease (CKD)
FLD is an independent risk factor for CKD. Mechanisms include:
- Systemic Inflammation: Chronic inflammation and oxidative stress contribute to kidney damage.
- Endothelial Dysfunction: Shared risk factors like insulin resistance and hypertension promote renal dysfunction.
4. Endocrine Disorders
FLD is associated with a number of endocrine disorders, including:
- Polycystic Ovary Syndrome (PCOS): Insulin resistance links FLD to PCOS, a common endocrine disorder in women.
- Hypothyroidism: Thyroid dysfunction, particularly hypothyroidism, is more prevalent in FLD patients and may exacerbate metabolic disturbances.
5. Sleep Apnea
Obstructive sleep apnea (OSA) is frequently observed in FLD patients. The pathophysiological link is thought to involve shared risk factors, such as obesity, as well as systemic inflammation, which may contribute to airway collapse during sleep.
6. Malignancies
In addition to hepatocellular carcinoma (HCC), FLD has been associated with an increased risk of extrahepatic malignancies, including colorectal, breast, and pancreatic cancers. Chronic inflammation and altered immune surveillance are thought to underlie this increased cancer risk.
Conclusion
FLD is not merely a liver-specific disorder; it represents a systemic disease with far-reaching consequences. Fat deposition in the liver disrupts a range of hepatic functions, primarily through oxidative stress, inflammation, and insulin resistance. As FLD progresses, it not only impairs the liver’s ability to regulate metabolism, detoxify toxins, and synthesize essential proteins, but it also predisposes patients to a wide array of extrahepatic diseases, including cardiovascular disease, type 2 diabetes, chronic kidney disease, and various malignancies.
FLD has a variable prognosis, largely dependent on the amount of fat accumulated in the liver and the degree of fibrosis. While simple steatosis generally has a benign course, NASH can progress to cirrhosis in 15-20% of patients, with an increased risk of liver-related complications, including HCC. Cardiovascular disease (CVD) remains the leading cause of death in patients with FLD, highlighting the importance of managing associated metabolic disorders.
References
- Abenavoli, L., et al. (2016). Insulin resistance and liver steatosis: clinical and therapeutic implications. World Journal of Gastroenterology, 22(39), 8957-8970.
- Friedman, S. L., et al. (2018). Mechanisms of NAFLD development and therapeutic strategies. Nature Medicine, 24(7), 908-922.
- Targher, G., et al. (2018). Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. New England Journal of Medicine, 379(24), 2544-2555.