The Role of Nutrient Deficiencies and Liver Dysfunction
High cholesterol is a prevalent health issue that significantly increases the risk of cardiovascular diseases. It leads to the buildup of fatty deposits within arterial walls, a condition known as atherosclerosis, which can result in heart attacks and strokes. Emerging research suggests a strong interconnection between high cholesterol, impaired liver function, and nutrient deficiencies. These interconnections are a result of the pivotal role that specific nutrients play in maintaining both cholesterol levels and liver health.
High Cholesterol
Cholesterol is a fatty substance found in every cell of the body, essential for producing hormones, vitamin D, and substances that help digest foods. However, high levels of low-density lipoprotein (LDL) cholesterol can lead to the buildup of plaques in arteries, reducing blood flow and increasing the risk of cardiovascular events.
- LDL Cholesterol: Often referred to as “bad” cholesterol, high levels contribute to plaque formation in arteries.
- HDL Cholesterol: Known as “good” cholesterol, it helps remove LDL cholesterol from the bloodstream.
- Triglycerides: High levels of these fats in the blood also increase the risk of atherosclerosis.
The Role of the Liver in Cholesterol Metabolism
The liver plays a crucial role in managing cholesterol levels by producing, processing, and removing cholesterol from the body. It synthesizes bile acids from cholesterol, which are essential for digesting fats. Impaired liver function can disrupt these processes, leading to high cholesterol levels.
Liver Functions:
- Cholesterol Production: The liver produces about 80% of the body’s cholesterol.
- Bile Acid Production: Bile acids, derived from cholesterol, are crucial for fat digestion and absorption.
- Detoxification: The liver detoxifies various metabolites, including cholesterol by-products.
Nutrient Deficiencies and Liver Dysfunction
Nutritional deficiencies can severely impact liver function and cholesterol metabolism. Essential nutrients like choline, inositol, methionine, and taurine play significant roles in maintaining liver health and cholesterol balance.
Choline:
- Function: Essential for lipid metabolism and liver function.
- Deficiency Impact: Leads to fatty liver disease and impaired lipid transport, increasing blood cholesterol levels.
Inositol:
- Function: Vital for lipid metabolism and insulin signaling.
- Deficiency Impact: Disrupts fat metabolism, leading to increased cholesterol and triglycerides.
Methionine:
- Function: A crucial amino acid for methylation processes and detoxification.
- Deficiency Impact: Impairs liver’s ability to process fats, leading to elevated cholesterol levels.
Taurine:
- Function: Supports bile salt formation, crucial for fat digestion and detoxification.
- Deficiency Impact: Reduces bile production, impairing fat digestion and increasing cholesterol levels.
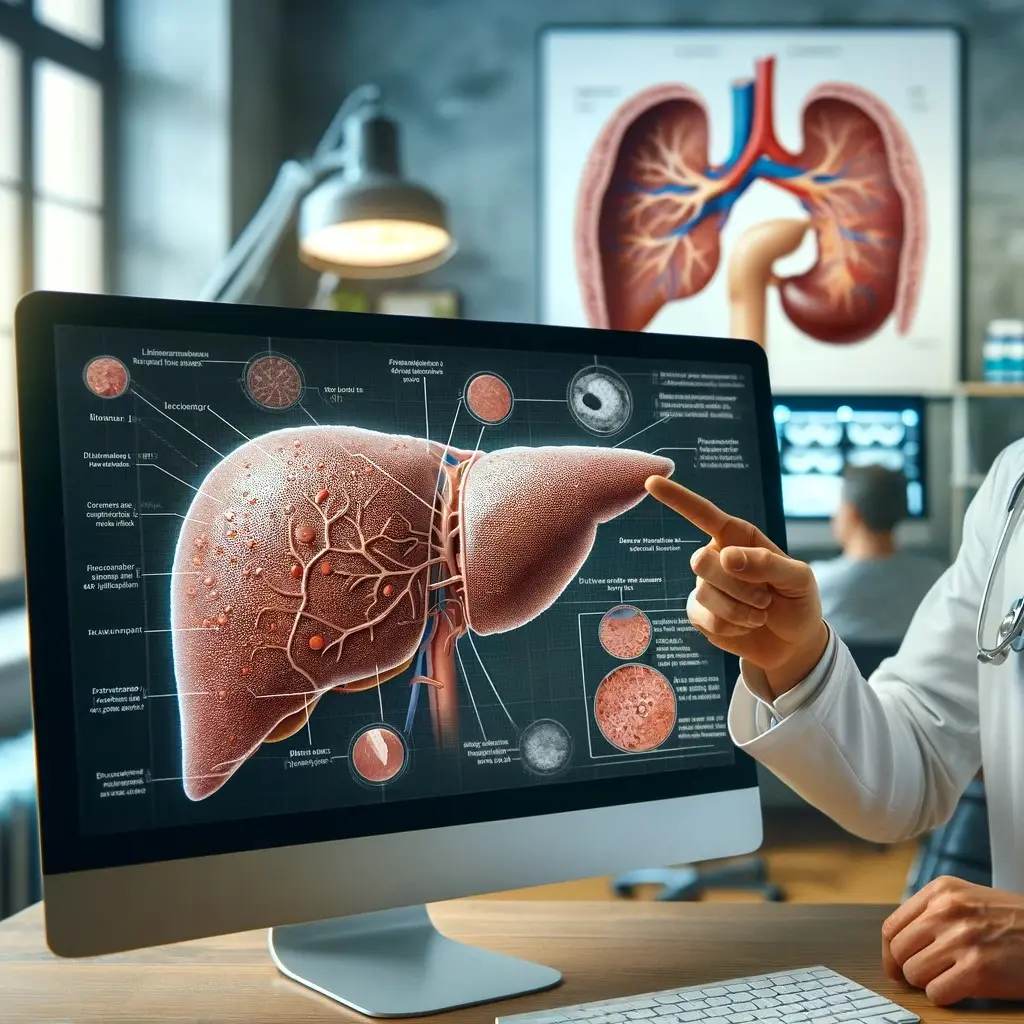
Interconnection Between High Cholesterol and Liver Dysfunction
The interrelationship between high cholesterol and liver dysfunction forms a feedback loop where each condition exacerbates the other.
Mechanisms of Interaction:
- Nutrient Deficiency: Deficiencies in choline, inositol, methionine, and taurine impair liver function.
- Liver Dysfunction: Impaired liver function disrupts cholesterol metabolism and bile production.
- High Cholesterol: Elevated cholesterol levels result from and further contribute to liver dysfunction.
- Cardiovascular Risk: The combined effect increases the risk of cardiovascular diseases due to plaque buildup in arteries.
Implications on Human Health
High cholesterol and impaired liver function due to nutrient deficiencies have extensive health implications:
Cardiovascular Diseases:
- Increased risk of heart attack, stroke, and peripheral artery disease due to atherosclerosis.
Liver Diseases:
- Progression from fatty liver disease to non-alcoholic steatohepatitis (NASH), cirrhosis, and liver cancer.
Metabolic Disorders:
- Development of metabolic syndrome, characterized by hypertension, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels.
Prevention and Management
Addressing nutrient deficiencies and improving liver health are crucial steps in managing high cholesterol:
Dietary Adjustments:
- Ensure adequate intake of choline, inositol, methionine, and taurine through a balanced diet and supplementation.
Regular Exercise:
- Physical activity helps improve liver function and cholesterol metabolism.
Limit Alcohol and Toxins:
- Reducing alcohol intake and exposure to toxins can prevent further liver damage.
Medical Consultation:
- Seek medical advice for proper diagnosis and treatment of high cholesterol and liver dysfunction.
High cholesterol is not just a standalone issue but is intricately linked to liver health and nutrient status. Ensuring adequate intake of essential nutrients like choline, inositol, methionine, and taurine is vital for maintaining liver function and managing cholesterol levels. By addressing these factors, individuals can significantly reduce their risk of cardiovascular diseases and improve overall health.
LiverGuard delivers Choline, Inositol, Methionine, and Taurine in HIGH DOSE, supporting a fast and safe liver regeneration process, which will help you improve your cholesterol profile.
References
- Zeisel, S. H., & da Costa, K. A. (2009). Choline: An Essential Nutrient for Public Health. Nutrition Reviews, 67(11), 615-623.
- Buchman, A. L., Sohel, M., Brown, M., Jenden, D. J., & Roch, M. (2001). The Effect of Choline Supplementation on Hepatic Steatosis in Patients Receiving Home Parenteral Nutrition. Hepatology, 34(3), 333-340.
- Beale, A., & Garcia-Perez, A. (2020). The Role of Inositol in the Treatment of Insulin Resistance. Clinical Therapeutics, 42(1), 63-72.
- Croze, M. L., & Soulage, C. O. (2013). Potential Role and Therapeutic Interests of Myo-Inositol in Metabolic Diseases. Biochimie, 95(10), 1811-1827.
- Finkelstein, J. D. (1990). Methionine Metabolism in Mammals. The Journal of Nutrition, 120(8), 1474-1477.
- Zeisel, S. H. (2006). Choline: Critical Role During Fetal Development and Dietary Requirements in Adults. Annual Review of Nutrition, 26, 229-250.
- Hayes, K. C., & Sturman, J. A. (1981). Taurine in Metabolism. Annual Review of Nutrition, 1, 401-425.
- Marcinkiewicz, J., & Kontny, E. (2014). Taurine and Inflammatory Diseases. Amino Acids, 46, 7-20.
- Targher, G., Corey, K. E., Byrne, C. D., & Roden, M. (2021). The Complex Link between NAFLD and Type 2 Diabetes Mellitus — Mechanisms and Treatments. Nature Reviews Gastroenterology & Hepatology, 18(9), 599-612.
- Kawanaka, M., Nishino, K., Nakamura, J., Urata, N., & Oka, T. (2021). Nutrient Deficiencies in Patients with Non-Alcoholic Fatty Liver Disease. Clinical Nutrition ESPEN, 41, 249-256.
- World Health Organization. (2020). WHO Guidelines on Physical Activity and Sedentary Behaviour.
- Day, C. P. (2006). From Fat to Inflammation. Gastroenterology, 130(1), 207-210.