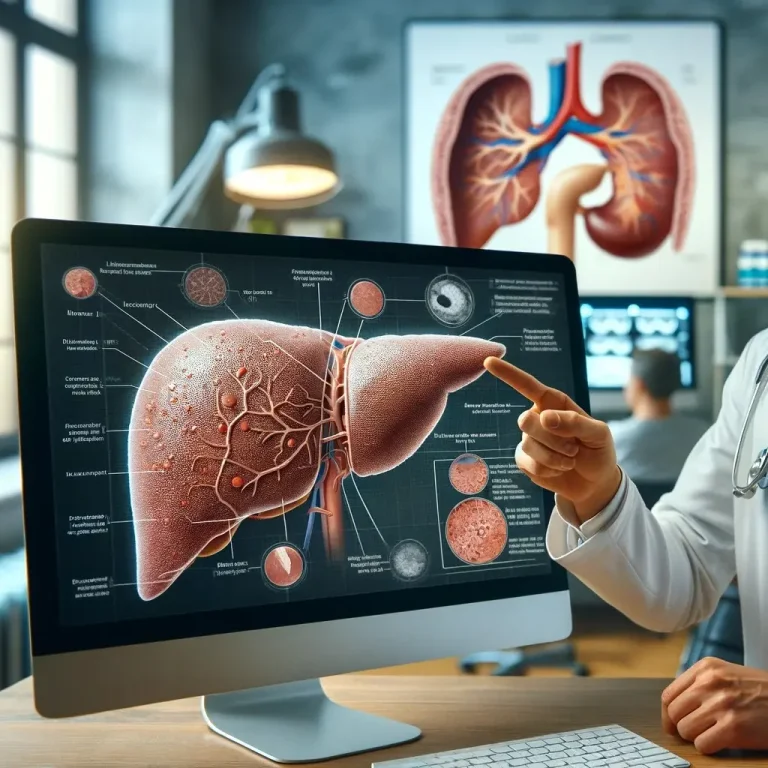
Liver self-recovery process
The liver has a remarkable ability to regenerate and repair itself, which is crucial for maintaining its essential functions. The self-recovery process of the liver involves several stages and mechanisms:
Cellular Regeneration
– Hepatocyte Proliferation: The primary cells of the liver, hepatocytes, have a high capacity for proliferation. When the liver is damaged, these cells can enter the cell cycle and begin to divide, replacing lost or damaged cells.
– Stem Cell Activation: In cases of severe damage where hepatocyte proliferation is insufficient, liver stem cells (also known as oval cells) can differentiate into hepatocytes or bile duct cells, aiding in tissue repair.
Inflammation Control
– Acute Response: Following liver injury, an acute inflammatory response occurs, involving the activation of Kupffer cells (liver macrophages) and other immune cells. This response helps to clear damaged cells and pathogens.
– Resolution of Inflammation: For effective recovery, the inflammatory response must be well-regulated. Anti-inflammatory signals and immune regulatory mechanisms ensure that inflammation subsides once the initial damage is addressed, preventing chronic inflammation that could lead to further tissue damage.
Extracellular Matrix Remodeling
– Matrix Degradation: The liver’s extracellular matrix (ECM) provides structural support. During injury, ECM components can become dysregulated. Matrix metalloproteinases (MMPs) are enzymes that degrade excess or damaged ECM components, allowing for proper tissue remodeling.
– Matrix Synthesis: Concurrently, fibroblasts and hepatic stellate cells produce new ECM components to support the regenerating tissue.
Angiogenesis
– New Blood Vessel Formation: Angiogenesis, the formation of new blood vessels, ensures that regenerating liver tissue receives adequate blood supply. This process is mediated by growth factors such as vascular endothelial growth factor (VEGF).
Growth Factor Signaling
– Proliferative Signals: Growth factors like hepatocyte growth factor (HGF), transforming growth factor-alpha (TGF-α), and epidermal growth factor (EGF) play critical roles in promoting hepatocyte proliferation and tissue repair.
– Regulatory Signals: Transforming growth factor-beta (TGF-β) and other signaling molecules help regulate the balance between cell proliferation, differentiation, and apoptosis, ensuring controlled regeneration.
Metabolic Reprogramming
– Energy Supply: Regenerating liver tissue requires significant energy and nutrients. Metabolic pathways are reprogrammed to prioritize energy production and biosynthesis needed for cell growth and division.
– Detoxification: The liver’s detoxification capacity is temporarily adjusted to accommodate the increased metabolic demands and the clearance of damaged cell components.
Essential Nutrients for Liver Regeneration
Nutrients that are essential are those that the body cannot synthesize on its own, or not in sufficient quantities, and therefore must be obtained from the diet. These nutrients are critical for normal body function and overall health.
For the liver self-regeneration processes they are Choline, Taurine, Inositol, and Methionine. All of them, provided by LiverGuard in HIGH DOSE contribute unique benefits that support hepatocyte health, lipid metabolism, and cellular repair mechanisms. Ensuring adequate intake of these nutrients through diet or supplementation can significantly improve liver regenerative capacity.
Functional Recovery
– Restoration of Liver Functions: As the structural integrity of the liver is restored, its functional capacities, including bile production, detoxification, protein synthesis, and metabolism, gradually return to normal.
The liver’s regenerative capacity is robust, but it is not limitless. Chronic or repeated damage, as seen in conditions like chronic hepatitis, alcohol abuse, or non-alcoholic fatty liver disease, can overwhelm the liver’s ability to repair itself, leading to fibrosis, cirrhosis, and eventually liver failure. Therefore, maintaining liver health through a balanced diet and supplementation, regular exercise, avoiding excessive alcohol consumption, and managing underlying health conditions is crucial for supporting its self-recovery processes and your overall health.
References
- Fausto, N., Campbell, J. S., & Riehle, K. J. (2006). Liver regeneration. Hepatology, 43(S1), S45-S53.
- Cohen, D. E., & Anania, F. A. (2011). Choline and liver disease. Current Opinion in Clinical Nutrition & Metabolic Care, 14(6), 575-581.
- McCuskey, R. S., et al. (1996). Role of the hepatic microvasculature in acetaminophen-induced hepatotoxicity. Microcirculation, 3(4), 367-379.
- Brass, E. P. (2002). Supplemental carnitine and exercise. The American Journal of Clinical Nutrition, 76(6), 1183S-1187S.
- Lieber, C. S. (1997). Ethanol metabolism, cirrhosis, and alcoholism. Clinical Chimica Acta, 257(1), 59-84.